HUTCHMED’s Scientist Advancing the Frontier of Drug Discovery
HUTCHMED is a large, publicly traded (Nasdaq/AIM:HCM;HKEX:13) pharmaceutical research powerhouse with approximately 900 research and development (R&D) staff. Dr Nelson Ng joined HUTCHMED following the launch of the Hong Kong lab in 2024. It may only have three Hong Kong-based researchers now, but the lab team Nelson leads plays a key role in supporting the launch of global Phase 1 clinical trials. They achieve this by working closely with colleagues based in Chinese Mainland and around the globe. From basic molecular discovery to testing and distributing approved medicines, their roster and importance are growing in the world of oncological research.
Sphere: Thank you for speaking to me today. Let’s get into it. As a Hong Kong secondary school student, getting into UC Berkeley’s Economics programme is no mean feat! But you gave it up to switch to biology. Why?
Dr Nelson Ng: As a kid, I enjoyed sports – especially football. I had good skills, but my stamina was weak. It haunted me throughout my childhood and teenage years. I didn’t know what was happening. It wasn’t until I was studying economics at UC Berkeley that I found out I had alpha-thalassemia. It’s an inherited blood disorder caused by mutations in the alpha-globin gene. My red blood cells are a lot smaller than normal and carry less oxygen; hence the weak stamina. So it led me to the field of human genetics. If I could make scientific contributions to the health of human beings, I could fulfil my career achievement and build my self-esteem.
Sphere: Set on research, where did life take you after your Berkeley undergrad?
Ng: Leaving California behind, I stepped up to an MPhil degree in biochemistry at the Chinese University of Hong Kong, focusing on genetic diseases. That led to my PhD studies: a joint degree between HKU and King’s College London, followed by five years of post-doc training. My HKU supervisor was a clinical professor. [Clinical research] has to have some translational value [i.e., practical application]. By contrast, my King’s College thesis adviser was a dedicated scientist. From him, I received hardcore training in molecular technologies, including lab techniques and data analysis.
Sphere: What’s the most exciting part of your work?
Ng: Surprisingly, the failures! It’s not simply about the discovery of new data. When experiments fail, you learn and use the data to generate new hypotheses. This can suggest which new tumour subtypes might be effective or expand our tumour spectra.
Sphere: Is solo research different from working in a private sector research firm?
Ng: Very. It’s collaborative, project-based research. There are many cross-functional meetings with different functional teams at HUTCHMED. The chemistry and biologics teams create the structures of the drugs. Then we have the oncology biology and toxicology team. Then the translation medicine team. All the way to the DMPK [drug metabolism and pharmacokinetics, a field in drug development that studies how the body affects a drug and vice versa] perspective and on to testing the drugs in a clinical setting by our medical science and clinical operation teams.
These functional teams integrate to ensure that our drug can enter clinical trials and become commercially available in the future. Knowing how the drug is developed from scratch to the final selling process is something that the company prepared me for. Also, knowing the limitations of each cross-functional team allows me to understand the entire process and how my department can help other teams.
Sphere: Is there a broad strategic approach to HUTCHMED’S research that is different from other research firms?
Ng: Compared to others, we have a very broad spectrum of pipelines.
One approach is the “safe options” approach, developed by harvesting well-established targets. We design the molecular structures of those inhibitors with specific properties which make our drug the best in its class.
Many molecular targets are known to be effective for specific tumour subtypes. For example, VEGFR (vascular endothelial growth factor receptor) inhibitors, which block tumour growth by suppressing blood vessel development, are already on the market. We improve the structure of these inhibitors to make them more potent and less toxic. That’s how we win the battle against competitors. Our first product, fruquintinib, is now approved around the globe in more than 30 countries, including major markets such as China, the US, Europe and Japan. That’s the first approach.
The second approach involves cutting-edge technologies, such as our ATTC platform [see explainer below], which enables us to discover completely new lines of attack for cancer treatment. The ATTC platform’s work is first-in-class; this means new innovations that have not yet been explored or validated by other players in the industry.
This ATTC platform is one of the most important projects we are currently working on. The development of the platform enables us to look at a wide range of molecular targets to address various challenges in cancer treatment. I’m assigned to a biomarker strategy team working on ATTC drugs. A biomarker strategy is like having a roadmap for using biological clues for making smarter healthcare choices, improving diagnosis and treatment, and monitoring diseases in a clear, organised way.
ATTC explained
An ATTC, or antibody-targeted therapy conjugate, is a cutting-edge cancer treatment that targets tumours with exceptional precision. Think of it as a smart delivery system: it combines a tiny drug (the small-molecule drug) with a special protein (the large-molecule antibody), held together by a connector called a linker. The antibody acts like a GPS, guiding the drug directly to tumour cells. Once inside the tumour, the drug detaches and begins its work to destroy the cancer cells.
In the past, other companies have created antibody-drug conjugates (ADCs), but the drug is a toxic agent that can harm both cancerous and healthy cells; effective, but with many undesirable side effects.
With HUTCHMED’s ATTC platform, the drug is replaced with a highly selective targeted therapy that offers improved safety and efficacy. As a result, doctors can administer the treatment earlier in the treatment journey, at higher doses, for extended periods, and in combination with chemotherapy, giving patients a better chance of fighting cancer.
Sphere: Are there other unique lines of work you are doing?
Ng: We are also detecting tumour DNA circulating in blood plasma by using next-generation sequencing. When we are not able to extract fresh tumour samples from patients, we can now take less invasive blood samples [as metastasising tumour cells break off the tumour and circulate in the bloodstream]. Using newer platforms, we can look at all those biomarkers by analysing the patient’s blood plasma before and after treatment.
Sphere: How does the process begin and what does the development pipeline look like?
Ng: It’s all about literature research and concepts. We have regular review meetings to push all of our targets to our chemistry team. The chemistry team, after hearing our proposal, will try to make molecules that could be drug candidates that attack these targets in cancer cells.
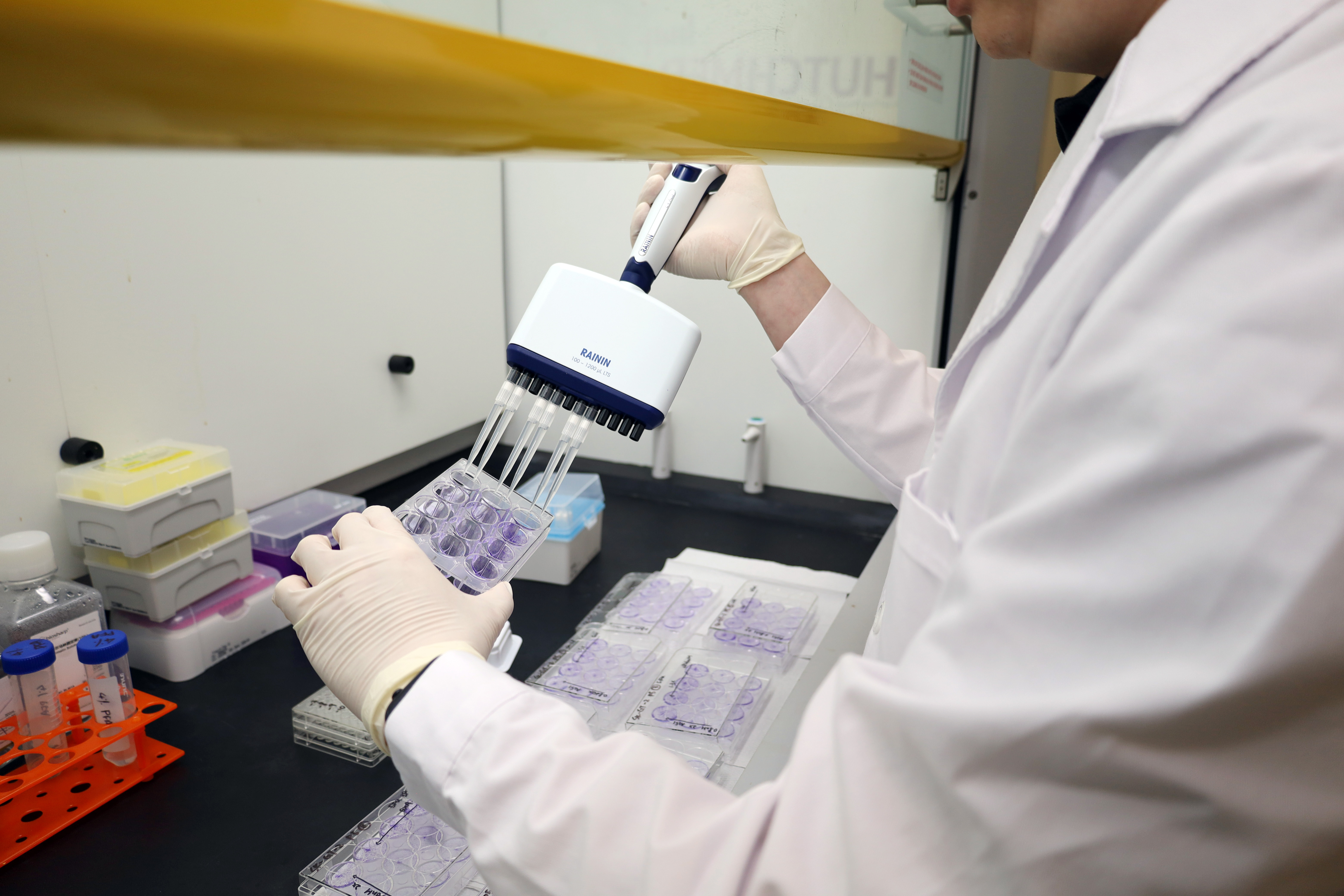
The chemistry team will generate multiple versions of drug candidates, after which the oncology team will screen these candidates to identify those with the highest potency in lab tests using cancer cells grown in Petri dishes. Then the in vivo [i.e. in live test subjects] teams will test a few of the most promising drugs in mice that have been implanted with tumour cells to see if we can observe a reduction in the tumour burden.
Sphere: A little more personal, is there life outside of research?
Ng: My hobby is wine tasting! I’m WSET* Level 2 qualified. As a scientist, you have to understand how a wine is made, which grape variety is used to make a wine, what the wine-making method is and much more. My favourite is the Châteauneuf-du-Pape from the Rhône region of France.
Sphere: While it’s good to know you are on the job helping to cure debilitating diseases, it’s good to know you know how to unwind as well! Thank you for sitting down with me today, and all the best as you grow the important HUTCHMED research presence in Hong Kong.
Ng: Thank you too!
*WSET: Wine & Spirit Education Trust, the world’s leading body for wine education, with a four-level qualification programme (four being the highest) denoting learning and expertise.